Abstract
Background: Although improvements have been made in understanding the pathophysiology of Acute Myeloid Leukemia (AML), heading to development of emerging therapies targeting leukemic stem cells, relapse is still a major problem leading to poor long-term survival and low cure rates. Of particular interest, Natural Killer (NK) cells are regulated by opposing signals from receptors that activate and inhibit effector function and are known to mediate anti-leukemic immunosurveillance in AML, but the mechanisms underlying the control of hematopoietic neoplasms by NK cells remains unclear and not yet explored as therapeutical options.
Aims: We hypothesized that functionally impaired NK cells due to imbalanced expression of inhibitory and activating receptors can predict poor outcomes in AML.
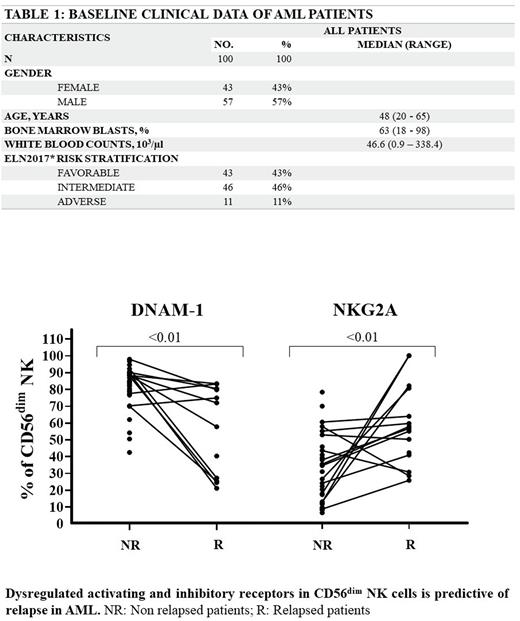
Methods: NK cell phenotypes based on the expression of DNAM-1 and NKG2D (activating) and NKG2A and KIR2DL1 (inhibitory) receptors on CD56+, CD56bright CD16- and CD56dim CD16+ NK subsets were profiled by multiparametric flow cytometry in 100 de novo AML bone marrow (BM) samples (Table 1), followed up from February 2016 to June 2022 and 17 healthy bone marrows (HBM). Correlations between NK phenotype with ELN2017 risk stratification, complete remission (CR), relapse (R), measurable residual disease (MRD), overall survival (OS) and relapse-free survival (RFS) were verified. Six BM from AML patients in remission after induction chemotherapy (AML-CR) were used to evaluate NK cell frequency and receptors recovery. Co-culture of AML-exposed CD56+ NK cells and K562 cell line was used to assay for killing (1:1, 5:1, 10:1 E:T ratios) and degranulation (CD107a). Mann Whitney, Kruskal-Wallis and mixed effects tests were performed to determine associations, and Log Rank test and Kaplan Meir curves were used for survival analysis.
Results: The frequency of all NK cell subsets were decreased in AML (P < .01). AML CD56+ NK cells showed decreased expression of NKG2D (P < .01), a trending to decreased DNAM-1 and increased NKG2A (P = .04) and KIR2DL1 (P < .01), while recovering to near healthy values in AML-CR. Expression of both NKG2D and DNAM-1 activating receptors was decreased (P < .01), while inhibitory NKG2A (P = .02) and KIR2DL1 (P < .01) were considerably increased in CD56dim NK, which is known to carry out the most cytotoxic activity. The expression of both activating receptors by CD56dim subset was found to be decreased in ELN2017 adverse versus low/intermediate risk (NKG2D, P = .05; DNAM-1, P < .01), in relapse (P < .01), and with similar trends in MRD+ patients after remission induction. The opposite was observed for inhibitory receptors, found to be increased in adverse risk (P < .01), relapse (NKG2A, P < .01; KIRDL1, P < .05) and MRD+ (NKG2A, P = .03) patients. Degranulation (P < .01) and specific target cell death (5:1, P = .01; 10:1, P = .002) were significantly decreased in AML. Patients with lower frequency of CD56dim NK expressing low NKG2D and DNAM-1 showed less degranulation and specific target cell death (P = .03), whereas patients with higher inhibitory receptors demonstrated lower degranulation (NKG2A, P=0.06) and cytotoxicity (KIR2DL1, P=.005). Of note, RFS was decreased in patients with lower frequency of CD56+ NK cells (P = .02) and both OS and RFS were decreased in patients with lower frequency of CD56dim NK cells (OS, P = .04; RFS, P = .03) and in patients with lower expression of NKG2D (OS, P = .03; RFS, P = .008) and DNAM-1 (OS, P = .02; RFS, P = .11) activating receptors, strongly suggesting an imbalance between activation and inhibition of NK cell activity.
Conclusion: Our data indicate that CD56dim NK show an exhaustion immunophenotype with high expression of KIR2DL1 and NKG2A inhibitory receptors and low expression of NKG2D and DNAM-1 activating receptors and that this imbalance leads to impaired cytotoxicity, compromised anti-leukemic activity and can be predictive of poor outcomes in AML, such as response to treatment, relapse and MRD positivity. Additionally, this NK phenotype at diagnosis could be considered an adverse risk prognostic factor associated with lower survival rates. Closing these gaps in the knowledge of NK-mediated immune evasion in leukemia is of significant interest for targeting the leukemic microenvironment by NK cell-mediated immunotherapy.
Disclosures
Costa:Novartis: Honoraria; Pfizer: Honoraria. Pagnano:Astellas: Consultancy, Honoraria; Wieth/Pfizer: Consultancy, Honoraria; GSK: Consultancy; Novartis: Consultancy, Honoraria. Traina:Novartis Pharmaceuticals Corporation: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal